Marital stress may impact young adults' recovery after a heart attack

- 1-11-2022, 08:58
- Participants reporting severe stress levels scored more than 1.6 points lower in physical health, and 2.6 points lower in mental health on a 12-item scale.
- Participants reporting severe stress levels reported almost 5 points lower in overall quality of life, and 8 points lower in quality of life when measured by a scale specifically designed for cardiac patients.
- Participants reporting severe marital stress were 67% more likely to report chest pains than people with mild or no marital stress. In addition, the likelihood of being readmitted to the hospital for any cause increased by almost 50% among those who reported severe marital stress.
- More women than men reported severe marital stress in their survey responses, with almost 4 out of 10 women reporting severe marital stress vs. 3 out of 10 men.
- All study findings persisted after accounting for sex, age and race or ethnicity; while the strength of association was reduced after socioeconomic factors, including education, income, employment and health insurance status were included in the analysis, the link remained statistically significant.
INA- sources
A stressful marriage may negatively impact heart attack recovery. Marital stress among younger adults (ages 18–55 years) was linked to worse recovery after a heart attack.
That negative impact did not change substantially after considering demographics and socioeconomic factors, such as education, employment, income and health insurance status, according to preliminary research to be presented at the American Heart Association's Scientific Sessions 2022.
The meeting, held in person in Chicago and virtually, Nov. 5-7, 2022, is a premier global exchange of the latest scientific advancements, research and evidence-based clinical practice updates in cardiovascular science.
According to the American Heart Association, heart disease including heart attack remains the leading cause of death in the U.S. An estimated 605,000 new heart attacks and 200,000 recurrent attacks happen in the U.S. each year.
Previous studies have found that psychological and social stress can lead to worse recovery from heart disease. While being married or partnered has been linked with better health and heart disease prognosis, what was unclear is if and how stress experienced in a marriage or romantic relationship (marital stress) may affect recovery after a heart attack, specifically among younger adults.
Zhu and colleagues compared recovery one year after a heart attack with self-reported marital stress. Study participants included 1,593 adults treated for a heart attack at 103 U.S. hospitals (located in 30 states across the country), who enrolled in another study called VIRGO, between 2008-2012.
All participants were either married or in a committed partnership at the time of their heart attack. Participants were average age of 47 years and included 1,199 (75.3%) white adults, 205 (12.9%) Black adults, 109 (6.8%) Hispanic adults and more than two-thirds were women.
To measure marital stress, at one month after a heart attack, participants completed a 17-item questionnaire called the Stockholm Marital Stress Scale (a scale previously developed and tested in elderly female cardiac patients in Stockholm, Sweden, which assesses marital stressors, including quality of the emotional and sexual relationship with the spouse or partner). Researchers classified participants based on their responses to the questionnaire into three groups: absent/mild marital stress, moderate marital stress or severe marital stress.
Participants were then followed for up to one year. Zhu and colleagues used a point scale to assess how participant's physical health may have limited his/her daily living activities, bodily pain and perceived health rating. The mental health component assessed participant's mental well-being and social interaction. Both stress and physical/mental health score were self-reported by the study participants. Hospital data was used to assess participant study eligibility and readmission data.
The analysis of the survey results compared with the hospitalization records indicate:
"Our findings support that stress experienced in one's everyday life, such as marital stress, may impact young adults' recovery after a heart attack. However, additional stressors beyond marital stress, such as financial strain or work stress, may also play a role in young adults' recovery, and the interaction between these factors require further research," Zhu said. "Future efforts should consider screening patients for everyday stress during follow-up appointments to help better identify people at high risk for low physical/mental recovery or additional hospitalization.
A holistic care model built upon both clinical factors and psychosocial aspects may be helpful, especially for younger adults after a heart attack."
"This study highlights the importance of evaluating the mental health of cardiac patients and is consistent with previous studies that show a greater burden of marital stress on the health of women," said Nieca Goldberg, M.D., American Heart Association expert volunteer, clinical associate professor of medicine at NYU Grossman School of Medicine and medical director of Atria NY. "A comprehensive approach to the care of cardiac patients that includes physical and mental health may transform the care of cardiac patients from the care of one organ to a patient's global health. The health care system should support the clinical assessment of both physical and mental health as that may lead to better outcomes and healthier lives for our patients."
Several limitations may have affected the study's results: the levels of marital stress and health outcomes were self-reported, therefore, self-perception may affect results, which may be inaccurate; it included patients in specific U.S. hospitals, so the results may not apply to people who live in other countries; and because participants were only followed for up to one-year after their heart attack, the results may not reflect long-term impact.
Co-authors are Rachel P. Dreyer, Ph.D.; Fan Li, Ph.D; Erica S. Spatz, M.D., M.H.S.; Cesar Caraballo-Cordovez, M.D.; Shiwani Mahajan, M.B.B.S., M.H.S.; Valeria Raparelli, M.D, Ph.D.; Erica C. Leifheit, Ph.D.; Yuan Lu, Sc.D.; Harlan M. Krumholz, M.D., S.M.; John Spertus, M.D., M.P.H.; Gail D'Onofrio, M.D., M.S.; Louise Pilote, M.D., M.P.H., Ph.D.; and Judith H. Lichtman, Ph.D. Authors' disclosures are listed in the abstract.
The current study was funded by Canadian Institutes of Health Research. The VIRGO (Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients) study was funded by the National Heart, Lung, and Blood Institute, a division of the National Institutes of Health.
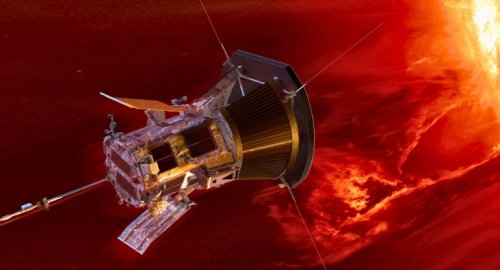
Parker Probe survives 'touching sun' in record-breaking flyby
- Multimedia
- 09:06
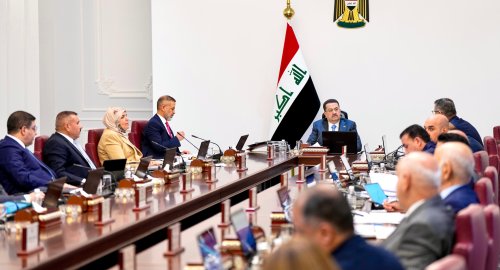
Full decisions of today's Cabinet session
- politics
- 09:06
Earthquake rattles north of Kirkuk, says MOT
- Local
- 08:08
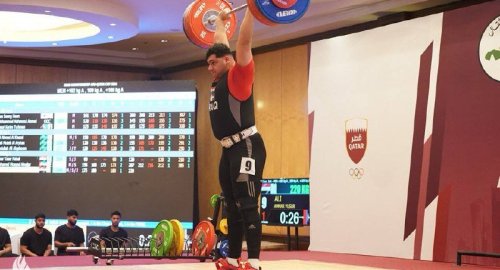
Iraq vs Saudi Arabia match kicks off, Arabian Gulf Cup 26
- Sport
- 24/12/28
Real Madrid becomes Arnold's new home
- Sport
- 24/12/28
Globe Soccer Awards 2024: all the nominees
- Sport
- 24/12/27